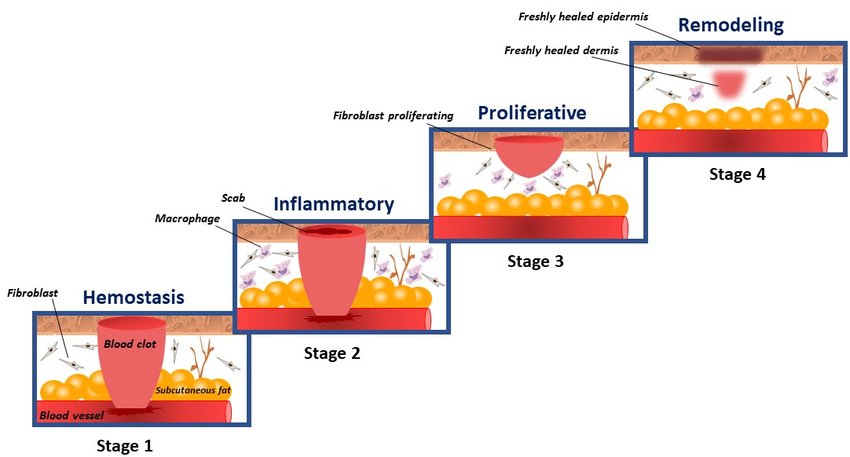
Wound Healing is a complex physiological process that involves a series of interconnected and coordinated steps to restore the structural and functional integrity of tissues after injury or trauma. The physiological mechanisms of healing can be divided into four main phases: hemostasis, inflammation, proliferation, and remodeling.
Health products can show healing efficacy, contributing to cell proliferation and tissue regeneration. In this article, we will address the physiological principles of this process and the molecular methodologies for validating healing efficacy.
Physiological stages of healing:
1. Hemostasis phase:
Hemostasis is the first phase of wound healing. It is the process that stops bleeding and starts the formation of a clot. During hemostasis, three steps occur:
- Vasoconstriction: Blood vessels in the injured area constrict, reducing blood flow. This helps to decrease blood loss.
- Clot formation: Blood platelets begin to accumulate at the wound site, forming a solid mass. Platelets release chemicals that activate other platelets, making the clot larger and more solid. Blood clotting proteins are also activated and help to stabilize the clot.
- Clot shrinkage: The clot begins to contract, reducing the size of the wound. This helps limit further blood loss and paves the way for the next phase of healing.
After hemostasis, the inflammatory phase begins, which involves the arrival of immune cells and growth factors that help repair the injured tissue.
2. Inflammatory phase:
The inflammatory phase of wound healing is characterized by an acute inflammatory response that occurs immediately after injury. The purpose of this phase is to remove damaged tissues and initiate tissue repair. Inflammation is mediated by immune cells, including leukocytes, macrophages, and dendritic cells, which are attracted to the site of injury. These cells help to remove cell debris, bacteria, and other foreign substances, thus starting the wound-cleaning process.
3. Proliferative phase:
At this stage, cells begin to proliferate and synthesize new tissue to replace damaged tissue. Fibroblasts are the key cells in this phase and are responsible for the synthesis of collagen and other extracellular matrix proteins, as well as the formation of new blood vessels. Angiogenesis is an important process in this phase, which involves the formation of new blood vessels to deliver nutrients and oxygen to growing cells. The proliferative phase can last several weeks or months, depending on the extent of the injury and the body’s ability to regenerate damaged tissue.
4. Remodeling phase:
In this final phase, the scar tissue begins to remodel and strengthen. Fibroblasts continue to synthesize collagen and other extracellular matrix proteins, but the concentration of these proteins begins to decrease and the organization of the matrix begins to become more structured. Scar tissue begins to contract and acquire mechanical characteristics similar to the original tissue. The maturation phase can last from several months to years, depending on the severity of the injury and the location of the scar tissue.
DOI: http://dx.doi.org/10.3390/app11041713
Validation methodologies
There are several methodologies for validating the healing efficacy of health products, which assess cell proliferation, viability, and migration. Important indicators of the product’s effectiveness in promoting the repair ability of injured tissues. Below we will discuss more details about some of the most used in vitro techniques: scratch test, MTT, BrdU, and NRU.
Wound healing (scratch test):
The Scratch assay, also known as the scraping assay or wound assay, is a widely used technique to assess cell migration and the ability to close wounds in vitro. In this assay, a wound is created on a cell monolayer grown in a culture dish, usually using a blunt tool such as a pipette or syringe tip.
The progression of healing is observed by observing wound closure over time. Cells at the edge of the wound begin to move towards the center of the wound, filling in the empty space left by scraping. The speed and efficiency of this healing process can be quantified using image analysis techniques.
Establishing adequate controls is important to validate healing through the Scratch-assay. For example, a group of untreated cells can be used as a negative control, while a group of cells treated with an agent that enhances cell migration can be used as a positive control. Also, it is important to repeat the experiment several times to ensure that the results are consistent.
In summary, the Scratch assay is a useful and widely used technique to assess cell migration and wound closure capacity in vitro. Proper validation of this technique involves including appropriate controls and replicating the experiment multiple times to ensure consistency of results.
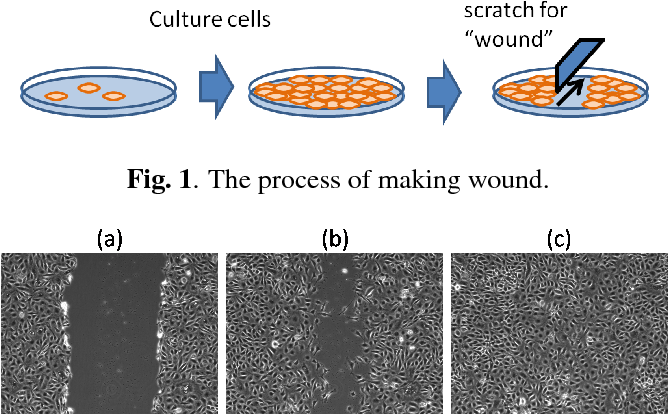
Ryoma Bise, et. al. 2010.
Cell cytotoxicity and proliferation (MTT, BrdU, NRU)
The MTT, BrdU, and NRU techniques are commonly used in cytotoxicity and cell proliferation studies to assess the healing efficacy of substances or materials.
- MTT Assay
The MTT technique (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) assesses cell viability and mitochondrial activity and is based on the conversion of tetrazolium salt to water-soluble formazan by living cells. The amount of formazan produced is proportional to cell viability and can be quantified spectrophotometrically.
The MTT technique does not directly assess the physiological mechanisms of healing, but cell viability and mitochondrial activity in cell culture, which are indirect indicators of the healing efficacy of a substance or material.
Cell viability is important in healing, as living cells are needed to replace injured tissue. Mitochondrial activity is important because mitochondria are responsible for producing the energy needed by cells to repair injured tissues.
Thus, the MTT technique can be used to assess the effectiveness of a substance or material in preserving cell viability and mitochondrial activity in cells involved in wound healing. Furthermore, it can be used to assess the cytotoxic potential of a compound, which can impair healing and lead to complications in the healing process.
Therefore, although the MTT technique does not directly assess the physiological mechanisms of healing, it can provide useful information about the healing effects of a substance or material. Other techniques, such as histological analysis and gene expression profiling, can be used in conjunction to directly assess the physiological mechanisms of wound healing.
- BrdU
The BrdU (bromodeoxyuridine) technique is used in cell proliferation studies and can be applied to validate healing efficacy. BrdU is a thymidine analog incorporated into the replicating DNA of proliferating cells, thus allowing the identification of cells that have undergone cell division.
In evaluating healing efficacy, the BrdU technique can be used to assess the rate of cell proliferation in the wound area. The application of BrdU is made in conjunction with a fluorescent marker specific for BrdU, thus allowing the identification of cells that have undergone cell division.
- NRU
The NRU technique (Neutral Red Uptake) is used in the validation of healing efficacy through the evaluation of cell viability. This technique is based on the cell’s ability to absorb the Neutral Red dye, which accumulates in its lysosomes, and which, when in contact with acidic solutions, such as that of lysosomes, changes color, becoming red.
In the NRU technique, viable cells from the wound area are treated with the Neutral Red dye and, subsequently, with an acidic solution, which causes the release of the dye from the lysosomes. The released dye is then quantified by spectrophotometry and the measured absorbance is directly proportional to the number of viable cells present.
The NRU technique is a simple and quick way to assess cell viability, but it is important to emphasize that the NRU technique does not allow the differentiation between specific cells, such as inflammatory cells and epithelial cells, and does not provide information about the capacity for cell proliferation, which is an important measure in wound healing. Therefore, it must be used in conjunction with other techniques for a more complete assessment of healing efficacy.
The combination of these techniques can provide valuable information on cytotoxicity and cell proliferation in healing efficacy studies, allowing assessment of both viability and cell activity in the presence of healing products, and validating their effectiveness.
Crop Approach
Crop Biolabs is an integrated external R&D facility, specializing in a variety of preclinical and analytical services, external quality assessment, phenotypic and molecular assays for advanced therapeutics, pharmaceuticals, cosmetic ingredients, and sanitizing companies, in addition to providing claim substantiation and safety evaluations from discovery to regulation for new solutions and bespoke products.
We validate the healing effectiveness of health products through the scratch test and MTT, BrdU, and NRU techniques, with a personalized, agile, and cost-effective work plan.
Our mission is to collaborate with the technological maturation of products and developments in life sciences, either with a punctual service or with a complete R&D solution: from idea to impact.
Learn more about Crop Biolabs: https://cropbiolabs.com.br/
Author: Carolina Barizan, Biomedical Scientist – Marketing Analyst, Crop Biolabs